4 Things You Need to Know Before Quitting Ozempic, Says an Obesity Expert

Have you considered quitting Ozempic because of nausea, fatigue, or other uncomfortable side effects? You're not alone. Many patients struggle during their first weeks or months on GLP-1 medications. Dr. Meghan Garcia-Webb, a Boston-based physician board-certified in Internal Medicine, Lifestyle Medicine, and Obesity Medicine, has guided hundreds of patients through their weight loss journeys. She shares four essential insights that could transform your experience and help you achieve the results you're looking for before you decide to stop your medication.
1: Know When to Seek Emergency Care
Your safety is the absolute priority when taking Ozempic or other GLP-1 medications. Dr. Meghan emphasizes that ruling out medical emergencies must come first when experiencing severe side effects. "Pancreatitis, gastroparesis, bowel obstruction, gallbladder issues, gallstones—there are a lot of serious medical issues that can happen with these medications," she explains to her patients. Though these complications are rare, they require immediate medical attention.
"The number one thing is you have to make sure that people are not having a medical emergency," Dr. Meghan stresses in her practice. "I have to make sure they're eating, drinking, having bowel movements, urinating, like all the basic functions are happening."
Before assuming Ozempic is causing your symptoms, Dr. Meghan recommends considering other possible causes. "I would hate to blame things on the medication when maybe they have the flu or maybe they had food poisoning," she tells patients. "I've definitely had patients who started a supplement and they feel terrible around the same time and they feel awful, but then they stop the supplement and they feel better."
RELATED: 15 Things to Know Before Requesting Ozempic for Weight Loss
2: Understand Your Side Effect Pattern

Timing matters when it comes to Ozempic side effects. Dr. Meghan suggests tracking when your symptoms occur relative to your injection schedule. "Are you fatigued all the time, the whole week, or are you fatigued in the 24 to 48 hours after you take your injection?" she asks her patients.
Recognizing patterns helps manage expectations and plan your activities accordingly. "For some people it's like, it hits them on a particular day," Dr. Meghan explains. "They can kind of set their clock by it."
This awareness can make side effects more manageable. "If that's the case, sometimes that makes it a bit more manageable because then the patient knows what to expect," she tells them. "Actually I'm not tired all the time. I'm tired two days after I take my shot. And if I just plan around that, actually the rest of the week isn't so bad."
3: Prioritize Proper Nutrition

Reduced appetite is common when starting Ozempic, but proper nutrition remains essential. "The goal is not to become malnourished on these medications," Dr. Meghan cautions all her patients.
For those whose appetite decreases significantly, she has specific recommendations. "I always have to make sure that they're eating. I don't want people having three bites of food and calling it a day," Dr. Meghan shares in her consultations. "If people's appetite is really reduced when they first start it, I'm definitely having them start a multivitamin if they can tolerate it."
Dr. Meghan sometimes suggests temporary solutions. "I don't love protein shakes, but sometimes this is a helpful place to add it in short term because it can be a little more easy for people to get their nutrients that way," she explains. "You just have to be a little flexible, especially in the beginning."
RELATED: 20 Possible Ozempic Side Effects
4: Try These Medication Management Strategies

Before quitting Ozempic, Dr. Meghan recommends several proven strategies that have helped many of her patients continue their treatment successfully. Some patients tell her about severe side effects that lead them to consider stopping. One patient reported, "I'm constantly constipated and throwing up. Please be very careful if you take these medications." Another experienced "bad shivers, not feeling great week two," and contemplated quitting.
A third patient shared that after seven months, they were still struggling significantly: "I've lost a lot of muscle and it's very devastating because it's difficult to do anything when you have zero energy and you're always nauseous. I'm down 40 pounds, but with the muscle loss, it's not worth it."
Dr. Meghan acknowledges these medications come with serious effects. "They are serious medications with serious side effects and are definitely not something to be taken lightly or casually," she emphasizes. "My heart goes out to you because we hear a lot about how great they are, but they are serious medications."
Add Supportive Medications

Anti-nausea medication and other treatments can make a significant difference for Ozempic users. "Is this a patient who's going to do well with some Zofran on hand, some anti-nausea medication?" Dr. Meghan considers when helping patients. "Is this a person that we should think about adding some medication for acid reflux? Is this a person that maybe needs some Imodium for diarrhea or a short-term laxative?"
She evaluates which "as needed" medications would really benefit each patient. For long-term use, she asks, "How often are you using them? How much of a burden is this for you?"
RELATED: What Happens to Your Body When You Stop Taking Ozempic
Try a Slower Titration

Rushing to higher doses of Ozempic isn't always beneficial. "It's not a race," Dr. Meghan emphasizes to her patients. "I'm just going to keep somebody at the dose they're at or lower the dose. Just keep them there for a little while. Give their body a little bit more time to adjust, catch up, see where they're at."
This approach often yields results. "Maybe the side effects go away. And then maybe we try again, or maybe we just keep them at the lower dose," she explains. "Extending the time or bumping the dose down can be very helpful."
Consider Extended Intervals

Spacing out Ozempic doses can provide relief while maintaining benefits. "Sometimes I'll have them just do the dose every 10 days instead of every week and see if that makes things a little bit easier in the short term as well," Dr. Meghan shares with patients experiencing significant side effects.
This simple adjustment gives the body more time between doses to recover from side effects while still providing some therapeutic benefits.
RELATED: 20 Things to Avoid While on Ozempic
Switch Medications
Different GLP-1 medications may produce different side effect profiles for individual patients. "Sometimes I'll think about maybe changing them to a different GLP-1 medication," Dr. Meghan explains when Ozempic isn't working well.
This approach depends on practical factors. "This provided that their insurance will cover it, it's available. You know, all those logistical things, operational things are not a problem," she notes.
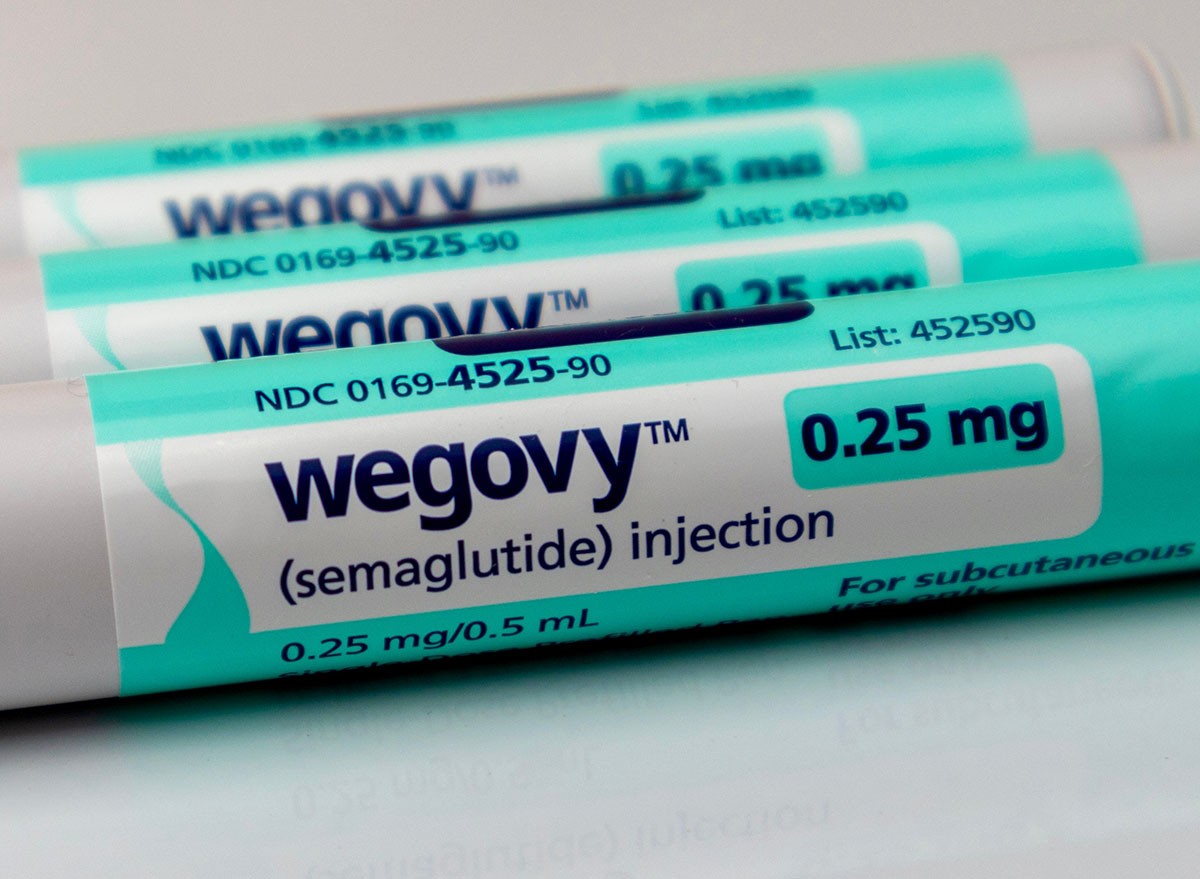
Dr. Meghan offers specific examples to her patients: "They're not doing well on Saxenda and maybe we should try Zepound or vice versa, or maybe we should try Wegovy instead of the Zepound."
When GLP-1 Medications Might Not Be Right for You

Sometimes, despite trying all four strategies, Ozempic or another GLP-1 medication simply isn't the right fit. "There are going to be those patients that I feel, they feel, we agree the medication is not a good fit for them for whatever reason," Dr. Meghan acknowledges.
This decision comes after thorough consideration. "They haven't been able to tolerate it. We've given it the amount of time that they can realistically give to it," she explains to patients. "Not all medication works well for everybody."
Dr. Meghan highlights this remains relatively uncommon. "That's going to be a very individual tailored discussion and decision," she explains. "Really, that's pretty rare on my end, but sometimes it's just not going to be a good fit. And that's okay. There are other options."
RELATED: 5 Foods That Maximize Weight Loss on GLP-1 Medicines, According to Coach
Talk to Your Doctor

The most important step is consulting with your doctor. "That's a good time to really have a more in-depth discussion with your prescribing physician as well," Dr. Meghan advises.
Remember, your weight loss journey is unique, and finding the right approach for your body might take time. Consulting with qualified medical professionals ensures you're making informed decisions about your health and well-being.




